Author -Dr Divya Shrinivas
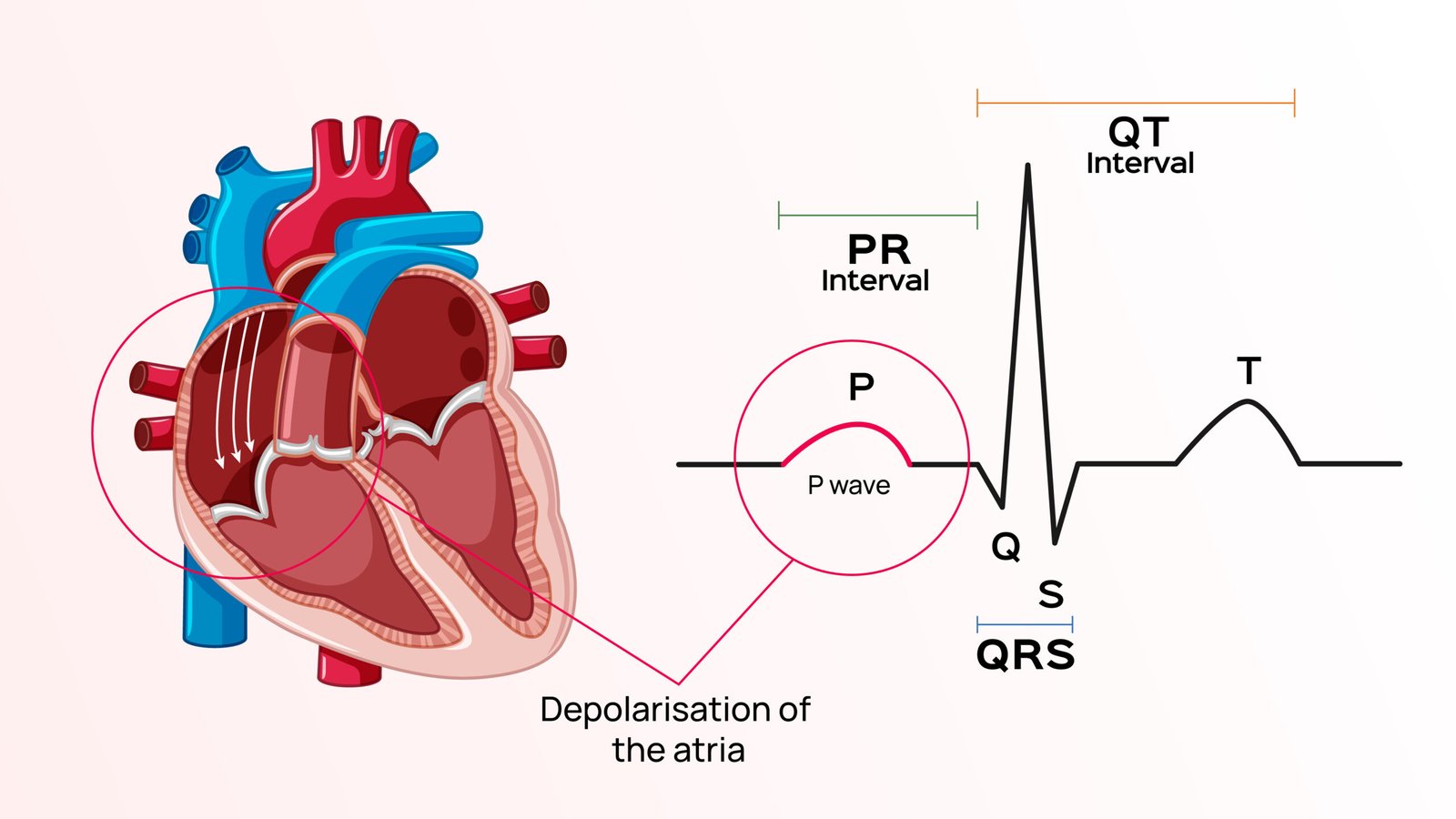
The P wave is an integral part of the Electrocardiogram (ECG). It is the first deflection from baseline voltage observed on an ECG. It represents the electrical depolarization of the atria of the heart, which is the orderly passage of electrical current sequentially through the heart muscle leading to the contraction of the heart. The normal duration of the P wave lasts less than 120 milliseconds (ms) or three small squares and less than 2.5 mm high on the ECG.
In a healthy person, the P wave originates at the sinoatrial node (SA node)- a small body of specialized muscle fibers, located in the right atrium of the heart, and disperses into both right and left atria. The early part of the P wave is formed due to the depolarization of the right atrium while the depolarization of the left atrium forms the middle and terminal portions of the P wave.
Abnormalities in the P wave
P wave abnormalities on an ECG generally point to a pathology in the atria of the heart. These abnormal ecg waves are most easily seen in the inferior leads (II, III and aVF) and lead V1, as the P waves are most prominent in these leads.
P mitrale (bifid P waves)
The presence of broad, notched (bifid) P waves in lead II is a sign of left atrial enlargement. This is because the left atrial depolarization lasts longer but the amplitude remains unchanged. Therefore the height of the resultant P wave remains within normal limits but the duration is more than 120 ms. A notch may or may not be present at the peak of the wave.
In the V1 lead of the ECG, left atrial enlargement leads to widening and deepening of the terminal negative portion of the P wave.
Left atrial enlargement can be caused by prolonged increase in pressure or volume in the left atrium. It is classically seen in case of mitral stenosis, which is the narrowing of the valve between the two left chambers of the heart. The narrowing of the valve makes it more difficult for the left atrium to pump blood into the left ventricle. This leads to increased pressure in the left atrium which inturn leads to enlargement.
Left atrial enlargement can also occur due to moderate and severe systemic hypertension. Prolonged hypertension can lead to hypertrophy of the left ventricle. The impairment in the flow of blood from the left atrium to the left ventricle due to increased ventricular stiffness causes left atrial enlargement. Left atrial enlargement can also be associated with aortic stenosis (narrowing of the valve between the left ventricle and the aorta which is the body’s main artery). Left atrial enlargement is a precursor to atrial fibrillation.
P pulmonale (peaked P waves)
Peaked P waves in lead II are seen in right atrial enlargement. The right atrial depolarisation lasts longer than normal and its waveform extends to the end of left atrial depolarisation. The amplitude of the right atrial depolarisation current remains unchanged but its peak falls on top of that of the left atrial depolarisation wave. This produces a P wave that is taller than normal (> 2.5 mm), but the width remains unchanged.
In the V1 lead of the ECG, right atrial enlargement causes increased height of the initial positive deflection of the P wave.
Right atrial enlargement can be caused by Congenital heart disease (conditions of the heart that have been present since birth), tricuspid stenosis (narrowing of the valve between the two right chambers of the heart leading to increased pressure on the right atrium causing its enlargement) or chronic lung disease. In patients of chronic obstructive pulmonary disease (COPD), there is an increase in pulmonary artery pressure which makes it difficult for the right ventricle to pump blood into it. This leads to right ventricular hypertrophy and can further cause right atrial enlargement. This can ultimately cause right heart failure called cor pulmonale.
P waves can be a combination of the above wave forms in case of biatrial enlargement.
Inverted P waves
P-wave inversion in the inferior leads that are II, III, aVF leads indicates a non-sinus origin of the P waves. When the PR interval is < 120 ms, the origin is in the AV junction, as seen in accelerated junctional rhythm (the automaticity of the AV junction increases while that of the SA node decreases). When the PR interval is ≥ 120 ms, the origin is within the atria as seen in ectopic atrial rhythm (when the origin is in the atria outside the sinus node)
Variable P wave morphology
The presence of multiple P wave morphologies indicates multiple ectopic pacemakers within the atria or the AV junction. If ≥ 3 different P wave morphologies are seen, then multifocal atrial rhythm is diagnosed. If ≥ 3 different P wave morphologies are seen and the rate is ≥ 100, then multifocal atrial tachycardia (MAT) is diagnosed. Multifocal atrial tachycardia is the rise of rapid, irregular atrial rhythm from multiple ectopic foci within the atria. It occurs in people with chronic obstructive pulmonary disorders or congestive cardiac failure.
Thus, abnormalities in the morphology of the P waves could indicate various pathologies of the heart. It is essential for clinicians to have an adequate understanding of ECGs to interpret these abnormalities, which would lead to timely diagnosis and treatment.



