Related Article
P wave ecg abnormalities and their role in cardiac wellness
QRS complex abnormalities: Clarifying ECG Abnormalities for Heart Health
pericarditis-symptoms-causes-and-treatment-explained
Protecting yourself against cerebrovascular disease
10 benefits of mango for heart patients
Author:- Mr. Ritesh Sharma
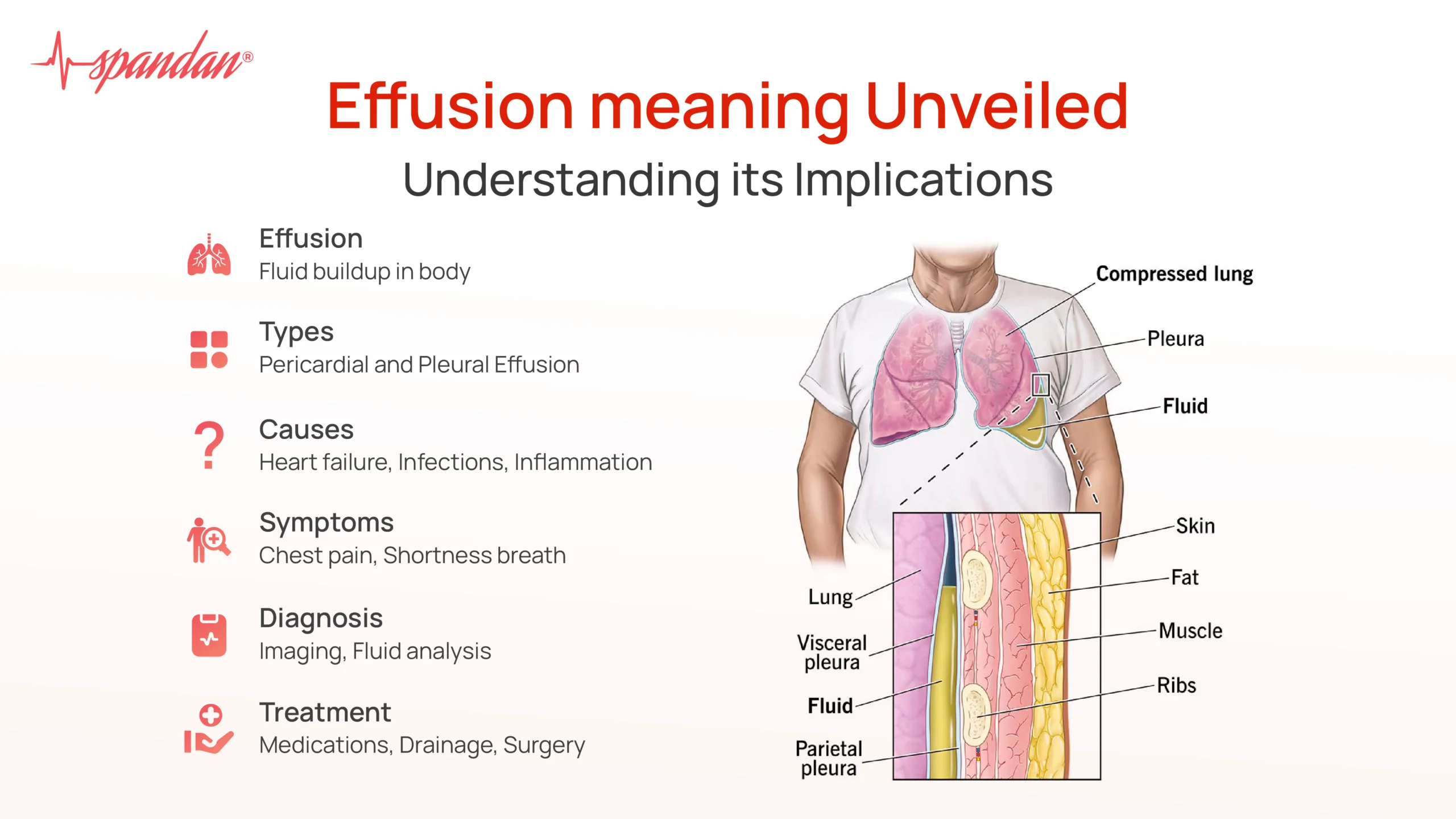
The effusion meaning has intrigued everyone in the field of healthcare for a very long time. From its traditional significance to its pivotal importance in the realm of heart health, the effusion meaning holds great significance. Before understanding effusion in the domain of cardiology, i.e. heart health, let’s try to understand the basic effusion meaning.
Effusion, a term originating from the Latin word “effusio” meaning “a pouring out,” is a critical concept in the medical field, especially concerning heart health. In cardiology, effusion typically refers to the accumulation of fluid in various parts of the body due to heart-related conditions. Hence, this makes it clear that both general people and clinicians must be aware of all the intricacies of this term. To understand the effusion meaning in cardiology, one needs to delve a little deeper into its medical implications. Therefore, we have crafted this blog.
This blog will cover all things related to the effusion meaning in the context of heart health. For this, we will discuss effusion meaning in cardiology, the types of effusion in cardiology- their symptoms and diagnosis, effusion causes and risk factors, implications for heart health, diagnosis and management, and treatment strategies. So, get ready to be educated and empowered by all knowledge regarding effusion meaning in all of its complexities.
Effusion Meaning in Cardiology
In the context of heart health, effusion generally refers to the abnormal accumulation of fluid in the pericardium (the sac surrounding the heart) or pleural spaces (the areas surrounding the lungs). The two primary types of effusion associated with heart conditions are pericardial effusion and pleural effusion.
Pericardial Effusion
Pericardial effusion occurs when excess fluid builds up in the pericardial cavity, the space between the heart and the pericardial sac. This condition can arise from various causes, including inflammation of the pericardium (pericarditis), infections, malignancies, autoimmune disorders, or as a complication of heart surgery.
Symptoms and Diagnosis
Patients with pericardial effusion may experience chest pain, shortness of breath, and a feeling of fullness in the chest. If the effusion is significant, it can lead to cardiac tamponade, a life-threatening condition where the pressure from the fluid restricts the heart’s ability to pump blood effectively.
Diagnosis typically involves imaging techniques such as echocardiography, which uses ultrasound waves to create images of the heart and detect fluid accumulation. Other diagnostic tools include chest X-rays, CT scans, and MRI.
Pleural Effusion
Pleural effusion refers to the buildup of fluid in the pleural space, the thin gap between the lungs and the chest wall. While pleural effusion can be caused by various conditions, heart failure is a common culprit. When the heart fails to pump blood efficiently, fluid can back up into the lungs and pleural space, leading to effusion.
Symptoms and Diagnosis
Symptoms of pleural effusion include shortness of breath, chest pain, and a persistent cough. As with pericardial effusion, imaging studies such as chest X-rays, ultrasounds, and CT scans are essential for diagnosing pleural effusion. Thoracentesis, a procedure where fluid is removed from the pleural space with a needle, can also help diagnose the underlying cause.
Causes and Risk Factors
Effusions related to heart health often stem from conditions that affect the heart’s ability to pump blood or cause inflammation around the heart. Key causes and risk factors include:
- Congestive Heart Failure (CHF): CHF is a leading cause of both pericardial and pleural effusions. When the heart is unable to pump blood effectively, fluid can accumulate in the lungs, abdomen, and pleural and pericardial spaces.
- Pericarditis: Inflammation of the pericardium can lead to pericardial effusion. This condition can be caused by infections, autoimmune diseases, or post-surgical inflammation.
- Myocardial Infarction (Heart Attack): A heart attack can damage the heart muscle, potentially leading to inflammation and fluid buildup in the pericardial space.
- Kidney Failure: Reduced kidney function can cause fluid retention and contribute to effusions.
- Infections: Bacterial, viral, and fungal infections can cause inflammation and fluid accumulation in the pericardium and pleural spaces.
- Malignancies: Cancers, especially those affecting the lungs or lymphatic system, can lead to effusions by obstructing fluid drainage or causing inflammation.
Implications for Heart Health
Effusions have significant implications for heart health. The presence of fluid in the pericardial or pleural spaces can compromise heart function and lead to severe complications.
Cardiac Tamponade
One of the most critical complications of pericardial effusion is cardiac tamponade. In this condition, the accumulated fluid exerts pressure on the heart, hindering its ability to fill properly with blood. This leads to decreased cardiac output, which can cause shock and, if untreated, be fatal. Symptoms of cardiac tamponade include severe shortness of breath, low blood pressure, and fainting. Immediate medical intervention is necessary to drain the fluid and relieve the pressure on the heart.
Respiratory Complications
Pleural effusion can lead to respiratory distress due to the compression of the lungs, reducing their ability to expand fully. This results in decreased oxygen exchange and can exacerbate symptoms of heart failure. Chronic pleural effusion can also lead to pleural thickening and decreased lung compliance, further impairing respiratory function.
Diagnosis and Management
Effective management of effusions related to heart health involves accurate diagnosis and addressing the underlying causes.
Diagnostic Approaches
- Imaging: Echocardiography is crucial for diagnosing pericardial effusion, while chest X-rays and CT scans are essential for detecting pleural effusion.
- Laboratory Tests: Blood tests can help identify underlying conditions such as infections, autoimmune disorders, or kidney dysfunction.
- Fluid Analysis: Analyzing the fluid obtained through pericardiocentesis or thoracentesis can provide valuable information about the cause of the effusion.
Treatment Strategies
- Medical Management: Treating the underlying cause of the effusion is paramount. This may involve diuretics for heart failure, anti-inflammatory medications for pericarditis, or antibiotics for infections.
- Procedural Interventions: For significant effusions, procedures such as pericardiocentesis (draining fluid from the pericardium) or thoracentesis (draining fluid from the pleural space) may be necessary. In severe cases, surgical interventions like pericardial window or pleurodesis might be required to prevent fluid reaccumulation.
- Monitoring and Follow-up: Regular monitoring through imaging and clinical evaluation is essential to assess the effectiveness of treatment and detect any recurrence of effusion.
In conclusion, it is utterly important to understand the effusion meaning in the domain of cardiology. It can lead to severe complications, so you must be aware of its symptoms and take the necessary action if and when required. Through appropriate diagnostic approaches and targeted treatments, healthcare providers can manage effusions effectively, improving outcomes and quality of life for patients with heart-related conditions.
Related Article
P wave ecg abnormalities and their role in cardiac wellness
QRS complex abnormalities: Clarifying ECG Abnormalities for Heart Health
pericarditis-symptoms-causes-and-treatment-explained
Protecting yourself against cerebrovascular disease
10 benefits of mango for heart patients



