Author:- Mr. Ritesh Sharma
Junctional Bradycardia is an important arrhythmia to study in the realm of cardiac care. It is a type of arrhythmia that both general people and clinicians must be aware of to opt for the correct treatment options and prevention strategies. Before understanding junctional bradycardia, let us try to understand what bradycardia actually is. Bradycardia is a type of cardiac arrhythmia (irregularities in the heart rhythm) that is characterized by a slow heart rate. The normal range of heart rate of an adult human being is 60 to 100 beats per minute. Therefore, in bradycardia, the heart rate tends to go lower than 60 beats per minute.
Junctional bradycardia is a type of bradycardia in which the heart rate goes below than the normal rate. However, there are other characteristics of this arrhythmia belonging to this arrhythmia classification that give it a unique identity. What are those characteristics? We shall find out in this blog. Here, we will examine everything associated with junctional bradycardia, including a basic definition, causes, clinical manifestations and diagnosis, implications for patient care, and more. So, get educated about junctional bradycardia in all of its complexities through this blog.
What is Junctional Bradycardia?
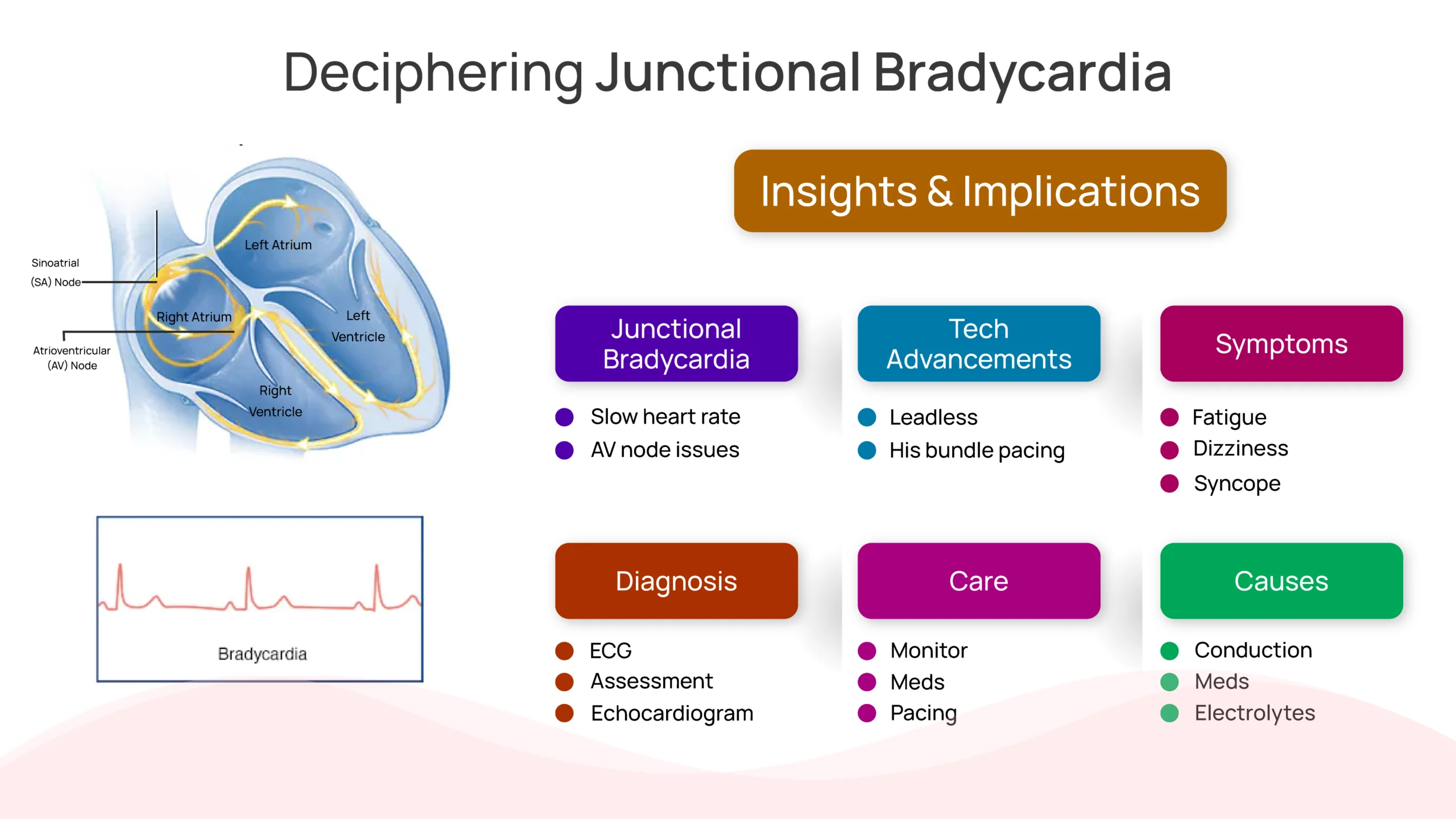
Junctional bradycardia refers to a cardiac arrhythmia characterized by a slow heart rate originating from the atrioventricular (AV) junction, i.e. an important part of the conduction system of the human heart. In a healthy heart, electrical impulses responsible for originating heartbeats originate from the sinoatrial (SA) node, often dubbed the heart’s natural pacemaker. These impulses travel through the atria, causing them to contract, and then reach the AV node, where they are relayed to the ventricles, resulting in ventricular contraction and subsequent pumping of blood to the body.
In junctional bradycardia, the electrical impulses either originate from the AV node or the surrounding tissues, bypassing the SA node. This results in a slower heart rate, typically below 60 beats per minute (bpm), which can lead to symptoms such as fatigue, dizziness, syncope (fainting), and even compromised cardiac output in severe cases.
Junctional Bradycardia Causes
There are several causes of junctional bradycardia mirroring the causes of junctional tachycardia. These causes include electrolyte imbalances, underlying conditions, medications, and more. Let’s learn about these causes in detail below:
- Cardiac Conduction System Disorders: Dysfunction within the cardiac conduction system, such as AV nodal dysfunction or damage to the AV node, can disrupt the normal propagation of electrical impulses, leading to junctional bradycardia.
- Medications: Certain medications, particularly those that affect the AV node or alter the balance of electrolytes in the body, can predispose individuals to junctional bradycardia. Examples include beta-blockers, calcium channel blockers, and antiarrhythmic drugs.
- Underlying Cardiac Conditions: Structural heart diseases, such as coronary artery disease, myocardial infarction, cardiomyopathy, and congenital heart defects, can disrupt normal cardiac conduction and contribute to junctional bradycardia.
- Electrolyte Imbalances: Abnormal levels of electrolytes, such as potassium, calcium, and magnesium, can impair cardiac conduction and predispose individuals to arrhythmias, including junctional bradycardia.
Clinical Manifestations and Diagnosis
Clinical manifestations of junctional bradycardia can vary depending on the severity of the arrhythmia and individual patient factors. Common symptoms include:
- Fatigue
- Dizziness
- Syncope (fainting)
- Shortness of breath
- Chest discomfort
Diagnosing junctional bradycardia typically involves a combination of clinical assessment, electrocardiography (ECG), and other cardiac monitoring modalities. On an ECG, junctional bradycardia is characterized by a slow heart rate with P waves that may be absent, inverted, or appear shortly before or after the QRS complex, so it shows P-wave ECG abnormalities. Additional tests, such as echocardiography, may be performed to evaluate for underlying structural heart disease.
Implications for Patient Care
It is important to know the implications for patient care for junctional bradycardia for its management and prevention. The treatment strategies for arrhythmia of this arrhythmia classification include:
- Observation and Monitoring: In asymptomatic patients with mild junctional bradycardia, a conservative approach involving regular monitoring and lifestyle modifications (e.g., avoiding triggers, maintaining electrolyte balance) may be sufficient.
- Medications: Pharmacological interventions, such as antiarrhythmic drugs or medications to correct electrolyte imbalances, may be prescribed to manage symptoms and stabilize cardiac rhythm.
- Cardiac Pacing: For symptomatic patients or those with severe junctional bradycardia refractory to medical therapy, cardiac pacing may be necessary. This involves implanting a pacemaker device to regulate the heart rate and ensure adequate cardiac output.
- Underlying Condition Management: Addressing underlying cardiac conditions, such as coronary artery disease or electrolyte disturbances, is essential in managing junctional bradycardia and preventing recurrence.
Advancements in Junctional Bradycardia Management
In the last few years, there have been several advancements that have helped manage junctional bradycardia. Let’s study about these technologies below:
- Leadless Pacemaker Technology: Traditional pacemaker devices require the implantation of leads (wires) into the heart via a transvenous approach, which can be associated with complications such as lead dislodgement, infection, and venous stenosis. Leadless pacemakers offer a minimally invasive alternative by eliminating the need for leads and utilizing a self-contained device directly implanted into the heart. These devices are particularly advantageous in patients with junctional bradycardia, providing reliable pacing without the risks associated with transvenous leads.
- His Bundle Pacing: Conventional right ventricular pacing, commonly used in pacemaker therapy, may result in dyssynchronous ventricular activation and adverse cardiac remodeling over time. His bundle pacing offers a physiologically more natural approach by stimulating the His-Purkinje conduction system, thereby preserving normal ventricular activation patterns. This technique has shown promising results in patients with junctional bradycardia, improving hemodynamics and reducing the risk of pacing-induced cardiomyopathy.
- Catheter Ablation: Radiofrequency catheter ablation has emerged as a therapeutic option for select patients with junctional bradycardia refractory to medical therapy or unsuitable for conventional pacing. By targeting and ablating abnormal conduction pathways or arrhythmogenic foci within the AV junction, catheter ablation can restore normal cardiac rhythm and alleviate symptoms. Although technically challenging and associated with procedural risks, catheter ablation offers the potential for long-term arrhythmia control and obviates the need for permanent pacing in some cases.
- Remote Monitoring Technologies: Remote monitoring systems allow healthcare providers to remotely assess device function, monitor arrhythmia burden, and detect clinical events in patients with pacemakers or implantable cardioverter-defibrillators (ICDs). These technologies enable early detection of arrhythmia recurrence or device malfunction, facilitating timely intervention and optimizing patient care. For individuals with junctional bradycardia requiring pacemaker therapy, remote monitoring offers enhanced surveillance and management of arrhythmia-related issues, improving patient safety and reducing healthcare resource utilization.
In conclusion, while Junctional Bradycardia can indeed be a dangerous arrhythmia to tackle, if you are affected by it, instead of fretting, you must opt for the correct treatment options. With the technological advancements, it is paramount to manage this arrhythmia which poses more danger than a normal arrhythmia such as heart palpitations. With a steadfast approach and rock-steady mindset, you can steer away from the implications of this arrhythmia and live a heart-healthy lifestyle.





