Author:- Mr. Ritesh Sharma
When we think of an electrocardiogram, we normally only discuss P-wave, QRS complex, and T-wave. However, there is another under-discussed ECG wave, i.e. osborn wave ECG. This ECG wave is also referred to as the J wave, much like other waves in the ECG waveform diagram showcased on the recording device, the J wave or Osborn wave ECG also has great significance within the domain of healthcare.
In this blog, we will cover all the facets of an Osborn wave ECG. For this, we will delve into its significance, causes, clinical implications, and interpretation. So, all healthcare professionals, who are not very familiar with Osborn wave ECG will get educated and enlightened through this blog.
What is an Osborn Wave ECG?
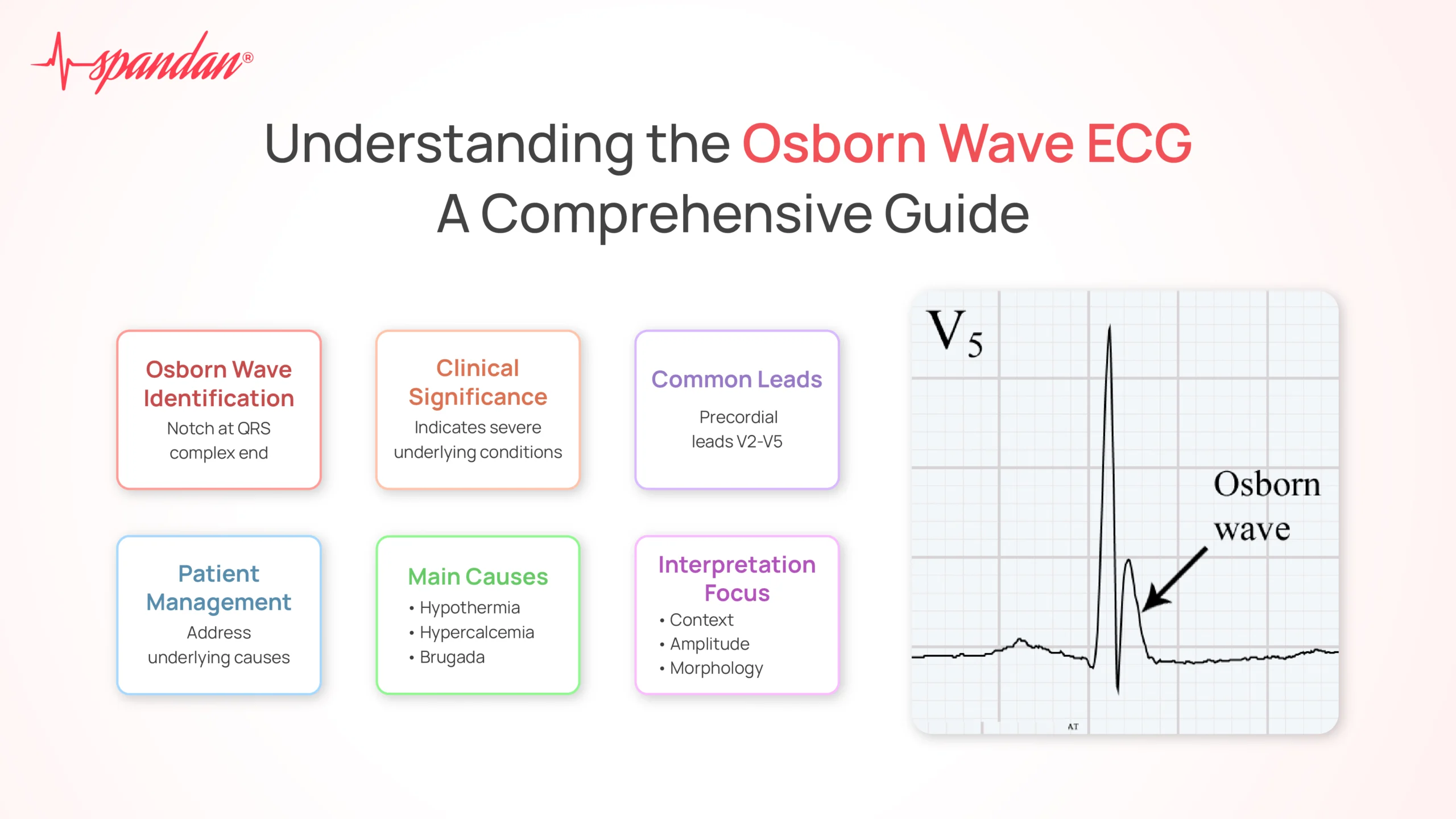
The Osborn wave is a deflection with a distinct notch at the terminal portion of the QRS complex on an ECG. Therefore, it can be classified in the QRS complex abnormalities. It was first described by Dr. John J. Osborn in 1953 during experiments on hypothermia in dogs. The wave is typically seen as a positive deflection, immediately following the R wave, before the onset of the ST segment.
Characteristics of the Osborn Wave ECG
- Appearance: The Osborn wave appears as a small upward notch at the end of the QRS complex. It is most commonly observed in the precordial leads, particularly V2 to V5.
- Amplitude: The amplitude of the Osborn wave varies and can be influenced by several factors, including the underlying cause and the degree of hypothermia. Larger waves are typically associated with more severe conditions.
- Duration: The wave is brief and can be easily missed if not specifically looked for. It typically merges into the ST segment.
Causes of the Osborn Wave ECG
The Osborn wave is associated with various conditions, primarily those that involve altered ion channel function in the heart. The most common causes include:
- Hypothermia: The classic and most recognized cause of the Osborn wave. As the body temperature drops, the risk of observing these waves increases, especially below 32°C (89.6°F).
- Hypercalcemia: Elevated levels of calcium in the blood can also lead to the appearance of Osborn waves. This condition requires careful monitoring and management to prevent cardiac complications.
- Brugada Syndrome: This genetic disorder affects the sodium channels in the heart and can lead to the appearance of Osborn waves. It is associated with a risk of sudden cardiac death and often requires intervention.
- Early Repolarization: Sometimes seen in healthy individuals, particularly athletes, where it is considered a benign finding. However, distinguishing it from pathological causes is crucial.
- Other Causes: Less commonly, the Osborn wave can be seen in conditions like ischemia, severe acidosis, or brain injury.
Clinical Implications
The presence of Osborn waves on an ECG can have significant clinical implications, depending on the underlying cause.
- Hypothermia: In hypothermic patients, the presence of Osborn waves indicates a severe drop in body temperature. Prompt rewarming and supportive care are critical to improving outcomes.
- Hypercalcemia: Recognition of Osborn waves in hypercalcemic patients can prompt immediate intervention to lower calcium levels, preventing potential cardiac arrhythmias.
- Brugada Syndrome: Identification of Osborn waves can lead to further investigation for Brugada syndrome, which might include genetic testing and consideration of implantable cardioverter-defibrillators (ICDs) for prevention of sudden death.
- Differentiating from Benign Causes: In athletes or individuals with early repolarization, distinguishing Osborn wave ECG from pathological causes can prevent unnecessary anxiety and interventions causing conditions like tachycardia.
Interpretation of the Osborn Wave ECG
Interpreting the Osborn wave requires careful analysis of the ECG in the context of the patient’s clinical presentation. Here are steps to consider:
- Clinical Context: Evaluate the patient’s symptoms and clinical history. Hypothermia, hypercalcemia, and known genetic conditions should raise suspicion.
- ECG Leads: Pay attention to the precordial leads (V2 to V5) where Osborn waves are more prominent.
- Wave Characteristics: Assess the amplitude and morphology of the wave. Larger waves suggest more severe underlying conditions.
- Differential Diagnosis: Consider other causes of similar ECG changes, such as ST-elevation myocardial infarction (STEMI) and pericarditis.
Management and Treatment
The management of conditions associated with Osborn waves involves addressing the underlying cause:
- Hypothermia: Rewarming techniques, both passive and active, are employed. Passive rewarming includes insulating the patient and preventing further heat loss, while active rewarming can involve warm intravenous fluids, heating blankets, or extracorporeal warming.
- Hypercalcemia: Treatments include intravenous hydration, bisphosphonates, calcitonin, and corticosteroids, depending on the severity and underlying cause.
- Brugada Syndrome: Management may involve lifestyle modifications, avoiding drugs that exacerbate the condition, and possibly the implantation of an ICD.
- Early Repolarization: Typically, no treatment is required unless associated with symptoms or other abnormalities.
In conclusion, though Osborn wave ECG is not discussed enough, it plays a pivotal role in the ECG test. With its clinical implications noticing this ECG test as an abnormal ECG during an ECG test is paramount for all healthcare professionals. Proper interpretation and management can significantly impact patient outcomes. By recognizing this unique ECG feature and correlating it with clinical findings, clinicians can ensure timely and appropriate interventions, ultimately improving patient care.



