Related Article
Author:- Mr. Ritesh Sharma
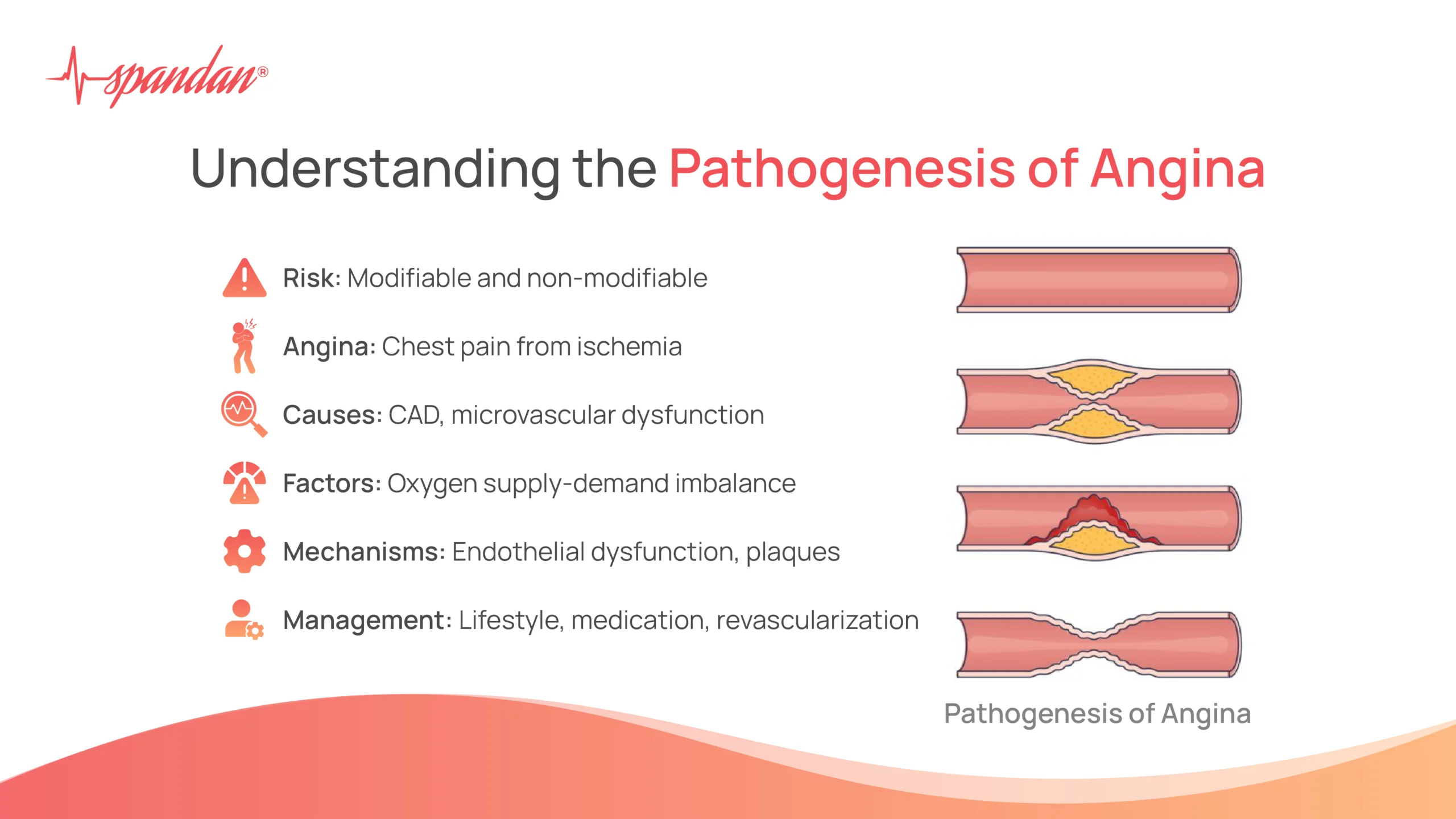
Angina pectoris, commonly known as angina, is a clinical syndrome characterized by chest pain or discomfort due to myocardial ischemia. Understanding the pathogenesis of angina is crucial for diagnosing, managing, and preventing this condition. This blog will delve into the intricate mechanisms underlying angina, exploring its causes, risk factors, and the physiological changes that lead to its development. So, all healthcare professionals and general people alike will get worthy insights through this blog.
What is Angina?
Angina is typically described as a squeezing, pressure-like pain in the chest that may radiate to the arms, neck, jaw, or back. It occurs when the heart muscle does not receive enough oxygen-rich blood to meet its needs, usually due to a partial or complete blockage of the coronary arteries. There are two main types of angina: stable angina and unstable angina.
Pathogenesis of Angina
The pathogenesis of angina involves multiple interconnected mechanisms that lead to myocardial ischemia. These mechanisms can be broadly categorized into factors affecting coronary blood flow, myocardial oxygen demand, and the balance between oxygen supply and demand.
1. Coronary Artery Disease (CAD)
Coronary artery disease is the most common cause of angina. It results from the buildup of atherosclerotic plaques within the coronary arteries, which can partially or completely obstruct blood flow. The pathogenesis of angina in CAD involves several stages:
- Endothelial Dysfunction: The initial step in atherosclerosis is endothelial dysfunction, where the inner lining of the arteries becomes damaged due to factors like hypertension, hyperlipidemia, smoking, and diabetes. This dysfunction leads to increased permeability to lipoproteins and an inflammatory response.
- Formation of Atherosclerotic Plaques: Lipoproteins, particularly low-density lipoprotein (LDL), penetrate the damaged endothelium and accumulate in the arterial wall. These lipoproteins undergo oxidation, triggering an inflammatory response. Macrophages engulf oxidized LDL, forming foam cells and creating fatty streaks, the precursors of atherosclerotic plaques.
- Plaque Progression and Complications: Over time, fatty streaks evolve into fibrous plaques, which consist of a lipid core and a fibrous cap. These plaques can grow and cause significant luminal narrowing. Plaques can also become unstable and rupture, leading to thrombosis and acute coronary syndromes, including unstable angina and myocardial infarction.
2. Imbalance Between Oxygen Supply and Demand
The pathogenesis of angina is also influenced by the balance between myocardial oxygen supply and demand. Several factors contribute to this balance:
- Increased Myocardial Oxygen Demand: Factors such as physical exertion, emotional stress, and high heart rate causing heart palpitations increase the heart’s oxygen demand. Conditions like left ventricular hypertrophy, aortic stenosis, and hyperthyroidism can also elevate oxygen demand.
- Reduced Myocardial Oxygen Supply: Besides atherosclerosis, other conditions can reduce coronary blood flow and oxygen supply, such as coronary artery spasm (Prinzmetal’s angina), anemia, hypoxemia, and microvascular disease.
3. Microvascular Dysfunction
Microvascular dysfunction, also known as coronary microvascular disease or syndrome X, involves abnormalities in the small coronary arterioles and capillaries. This condition can cause angina even in the absence of significant atherosclerotic plaques in the major coronary arteries. The pathogenesis of angina in microvascular dysfunction includes:
- Endothelial Dysfunction: Similar to CAD, endothelial dysfunction in the microvasculature can impair vasodilation and increase vascular resistance.
- Smooth Muscle Cell Dysfunction: Abnormalities in the function of smooth muscle cells in the microvasculature can lead to inappropriate vasoconstriction.
4. Coronary Artery Spasm
Coronary artery spasm, also known as variant angina or Prinzmetal’s angina, is caused by transient vasoconstriction of the coronary arteries. This spasm can occur in normal or atherosclerotic coronary arteries, reducing blood flow and causing angina. The pathogenesis of angina in coronary artery spasm involves:
- Hyperreactivity of the Vascular Smooth Muscle: Hyperreactive smooth muscle cells in the coronary arteries can lead to spasms.
- Endothelial Dysfunction: Impaired production of vasodilators like nitric oxide can contribute to coronary artery spasm.
5. Inflammation and Oxidative Stress
Inflammation and oxidative stress play crucial roles in the pathogenesis of angina by promoting endothelial dysfunction, plaque formation, and instability. Key aspects include:
- Inflammatory Mediators: Cytokines, chemokines, and other inflammatory mediators contribute to the development and progression of atherosclerosis.
- Oxidative Stress: Reactive oxygen species (ROS) can damage endothelial cells, oxidize LDL, and activate inflammatory pathways.
Risk Factors for Angina
Several risk factors contribute to the development of angina by influencing the pathogenesis of angina. These include:
- Non-Modifiable Risk Factors: Age, gender, and family history of coronary artery disease.
- Modifiable Risk Factors: Hypertension, hyperlipidemia, smoking, diabetes, obesity, sedentary lifestyle, and stress.
Clinical Implications and Management
Understanding the pathogenesis of angina is essential for its clinical management. Treatment strategies aim to reduce myocardial oxygen demand, improve coronary blood flow, and address underlying risk factors. Key approaches include:
- Lifestyle Modifications: Adopting a heart-healthy diet, regular physical activity, smoking cessation, and stress management.
- Medications: Anti-anginal medications (nitrates, beta-blockers, calcium channel blockers), antiplatelet agents (aspirin, clopidogrel), statins, and ACE inhibitors/ARBs.
- Revascularization: Procedures like percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) may be necessary for patients with significant coronary artery disease.
The pathogenesis of angina is a complex interplay of factors affecting coronary blood flow, myocardial oxygen demand, and the balance between supply and demand. Coronary artery disease, microvascular dysfunction, coronary artery spasm, inflammation, and oxidative stress all contribute to the development of angina. Understanding these mechanisms is crucial for effective diagnosis, management, and prevention of this condition. By addressing risk factors and implementing appropriate treatment strategies, patients with angina can achieve better outcomes and improved quality of life. If you or someone you know experiences symptoms of angina, seeking timely medical advice is essential for proper diagnosis and management.




