Author:- Mr. Ritesh Sharma
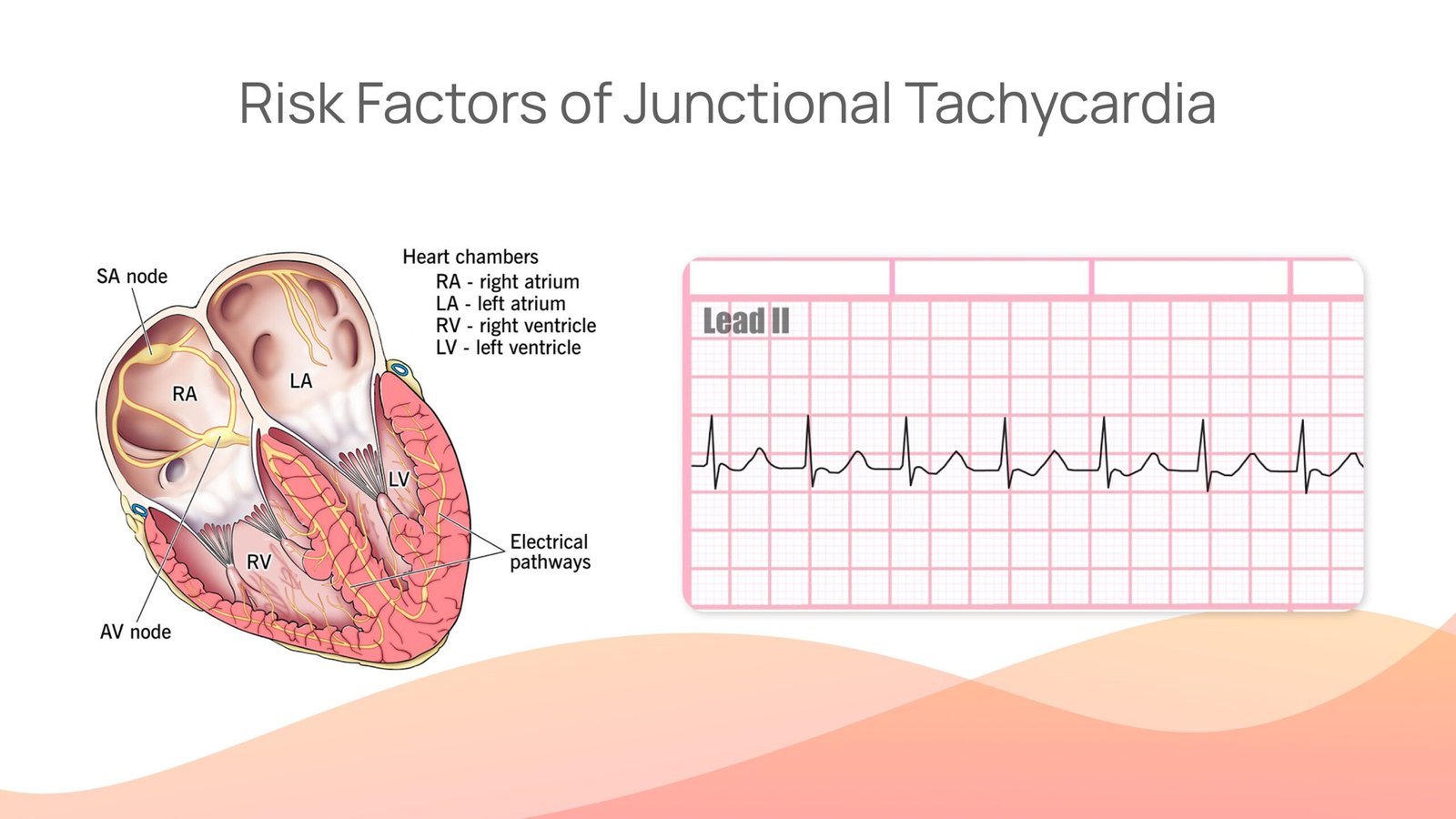
There are many arrhythmias (irregularities in the heart rhythm) that are characterized by rapid heartbeats. One of these arrhythmias is Junctional Tachycardia. This arrhythmia is a type of Supraventricular Tachycardia and is rare in the category because of its place of origin. Heart palpitations originating in the atrioventricular (AV) junction of the heart, define junctional tachycardia. The AV junction is the region of the heart between the atria and ventricles where the electrical signals are transmitted.
This tachycardia can occur in individuals suffering from structural heart disease. However, it can also be found in individuals without structural heart disease. There are various causes and risk factors of junctional tachycardia and it is a potentially harmful arrhythmia, but worry not, learning the specifics of it can certainly help in the timely detection and early prevention of it.
Junctional Tachycardia meaning
Junctional Tachycardia (also known as junctional ectopic tachycardia) is defined as a heart rhythm that starts from your heart’s natural pacemaker. Now, you must wonder, the natural pacemaker of the heart is the Sinoatrial Node (SA Node) from where the heartbeat originates and travels down through the heart. This is where the study of this Tachycardia becomes fascinating.
This arrhythmia occurs when the SA node is unable to start the heartbeat, therefore, the atrioventricular node replaces it. Now, the heartbeat originates from the junctions between the atria and ventricles as it has started posing as the natural pacemaker of the heart. Since the natural pacemaker of the heart is replaced, the normal sinus rhythm can no longer exist and the state of tachycardia arises, which is termed Junctional Tachycardia.
Normal heart rhythm vs. Junctional Tachycardia
The normal heart rhythm comes from the natural pacemaker of the heart, i.e. sinoatrial node. Therefore, the electrical impulses transmitted in the conduction process are normal, and the heart rate is 60 to 100 beats per minute. However, in the condition of junctional tachycardia, the heartbeat originates from the AV node which disrupts the whole conduction system. Hence, the heart rate in this case is above 100 beats per minute.
Types of Junctional Tachycardia
There are two types of junctional tachycardia. This arrhythmia is either prevalent in your body since birth or develops after surgery. Let’s discuss the types of junctional arrhythmia below:-
- Primary or congenital (since birth): This tachycardia is present in the body at the time of birth. Therefore, the heart of the baby beats 200 to 250 times per minute in the ventricles section, i.e. the lower chamber.
- Secondary or postoperative: This occurs more commonly than primary junctional tachycardia. In this arrhythmia, the child who undergoes surgery to fix a congenital heart problem develops this tachycardia.
Junctional Tachycardia Causes
Junctional Tachycardia has multiple causes. These causes range from heart conditions to genetic conditions. An elaborate and comprehensive study of all these causes is given below:-
- Heart Conditions:-
Heart Conditions such as structural heart disease, congenital heart defects, and acquired heart conditions can result in the development of this cardiac arrhythmia. - Cardiac Surgery:-
The procedures in cardiac surgery that involve AV junctions can sometimes lead to the condition of this arrhythmia. - Myocarditis:-
The inflammation of heart muscles (myocarditis) can disrupt the normal heart rhythm by making the electrical signal transmission chaotic. This can lead to various arrhythmias including this tachycardia. - Cardiomyopathy:-
The different forms of cardiomyopathy that influence the heart’s muscle structure can result in the development of junctional tachycardia. - Ischemic Heart Disease:-
Reduction in the blood flow to the heart’s muscle due to coronary artery disease can lead to junctional tachycardia. - Digitalis Toxicity:-
Medicines containing digitalis or digoxin which are prescribed for different conditions related to the heart can result in the development of junctional tachycardia. - Electrolyte Imbalances:-
The imbalances of electrolytes in the blood, for example, potassium, calcium, and magnesium can disrupt the electrical activity of the heart and lead to the condition of this tachycardia. - Hypoxia:-
If the oxygen level is low in the blood, it leads to a condition called chronic obstructive pulmonary disease (COPD). Apart from this, it can also cause severe respiratory distress, both these conditions can potentially cause tachycardia. - Infections:-
Infections such as endocarditis can disrupt the normal heart rhythm by causing inflammation which can result in the development of junctional tachycardia. - Medications:-
Some medications directly influence the heart’s conduction system which can potentially result in several arrhythmias, including junctional tachycardia.
Genetic Conditions:-
Genetic predisposition can sometimes lead to the development of arrhythmias. However, this happens in very rare cases.
Risk Factors for Junctional Tachycardia
The risk factors for junctional tachycardia rate can vary from individual to individual depending on age, gender, heart condition, etc. However, according to various studies, there are some common risk factors for arrhythmia. Let’s discuss these risk factors separately:-
- Heart Disease:-
Individuals with underlying heart diseases, such as coronary artery disease, myocarditis, or cardiomyopathy are likely to be affected more by junctional tachycardia. - Congenital Heart Defects:-
Some individuals are born with heart problems known as congenital heart defects, these heart defects can lead to junctional tachycardia and further worsen the state of the heart. - Myocardial Infarction (Heart Attack):-
Previous heart attacks can strain the heart’s tissue and lead to the disruption of normal heart rhythm which can further increase the risk of this tachycardia. - Age:-
Although junctional tachycardia can occur at any age, it poses more risk to older people due to changes in their heart’s electrical system. - Stimulant usage:-
Substances such as caffeine, nicotine, and illicit drugs can potentially stimulate the heart and trigger the risk of this arrhythmia.
Diagnosis of Junctional Tachycardia
The most potent way of diagnosing junctional tachycardia rhythm is an electrocardiogram (ECG/ EKG). The patients who are affected by the concerned arrhythmia will have a missing P wave which leads to p wave ecg abnormalities in the junctional tachycardia ECG which represents the starting of heartbeat from the SA node. Apart from this, the arrhythmia can also be identified by various other blood tests and echocardiography based on the medical history of the patient.
Hence, if you ever suspect junctional tachycardia, visit a healthcare professional and get your ECG and other tests done as soon as possible. If you are affected by the disease you will have an abnormal ecg.
Junctional Tachycardia Treatment options
The treatment options for junctional tachycardia depend on various factors. These factors are the severity of the arrhythmia, the medical conditions of the patient, and the underlying causes. Based on these factors different treatment options can be adopted by the patients.
- Observation and Monitoring:-
While this tachycardia can be a dangerous arrhythmia, healthcare professionals don’t immediately start treating it on detecting it. If the tachycardia doesn’t show major symptoms and is well-tolerated, the healthcare professionals first observe and monitor its severity.
- Vagal Maneuvers:-
Through vagal maneuvers, the healthcare professional stimulates the vagus nerve. Due to this, the instances of junctional tachycardia reduce or completely terminate. - Medications:-
To slow down the heart rate, doctors prescribe medicines such as beta-blockers, calcium channel blockers, or antiarrhythmic drugs like adenosine. These medicines are prescribed in accordance with the characteristics of the arrhythmia. - Cardioversion:-
If the medications prove to be ineffective for this tachycardia, healthcare professionals may adopt cardioversion. In this, the heart rhythm is restored using a controlled electric shock. - Ablation Therapy:-
When all other treatments fail to cure junctional tachycardia, healthcare professionals use catheter ablation. In this process, a thin, flexible tube (catheter) is placed into the heart at a target to destroy the abnormal tissue causing the damage. - Pacemaker Implantation:-
In very rare cases where junctional tachycardia causes slow heart rate, i.e. bradycardia, a pacemaker is implanted into the skin of the patient. This pacemaker sends electrical impulses to the heart when needed and regulates the heart rate. - Addressing Underlying Issues:-
If the arrhythmia is due to underlying issues, such as heart disease, infection, or electrolyte imbalance then they must be treated with the correct medications and procedures. - Modifications of Lifestyle:-
Along with the primary treatment, the healthcare professional also asks the patient to adopt some lifestyle modifications. These include reduction of intake of excessive caffeine, nicotine, or alcohol.
In conclusion, while Junctional Tachycardia can be hazardous to health, early detection and prompt medical interventions can save you from the risk of this arrhythmia. This type of Supraventricular Tachycardia can easily be cured if detected timely by identifying the prevalent symptoms.



