Author:- Mr. Ritesh Sharma
If you are a clinician, then you must be familiar with the term ventricular remodeling. This term is associated with the structural and functional alterations in the chambers of the human heart. As we all know, the human heart works tirelessly 24X7 to pump blood to all vital organs of the body. If we liken the human heart to machinery, then it is also likely to undergo some changes when responding to some stressors. These changes very much explain the concept of ventricular remodeling.
Whether you belong to the general audience or clinicians, ventricular remodeling is a fascinating topic to study. Therefore, through this blog, we will try to cover it in its entirety. For this, we will start with the definition of the condition, then delve into its mechanisms, causes, consequences, diagnostic evaluation, therapeutic strategies, and future directions. Hence, through this blog, you will be educated about ventricular remodeling in a thorough and elaborate manner.
What is Ventricular Remodeling?
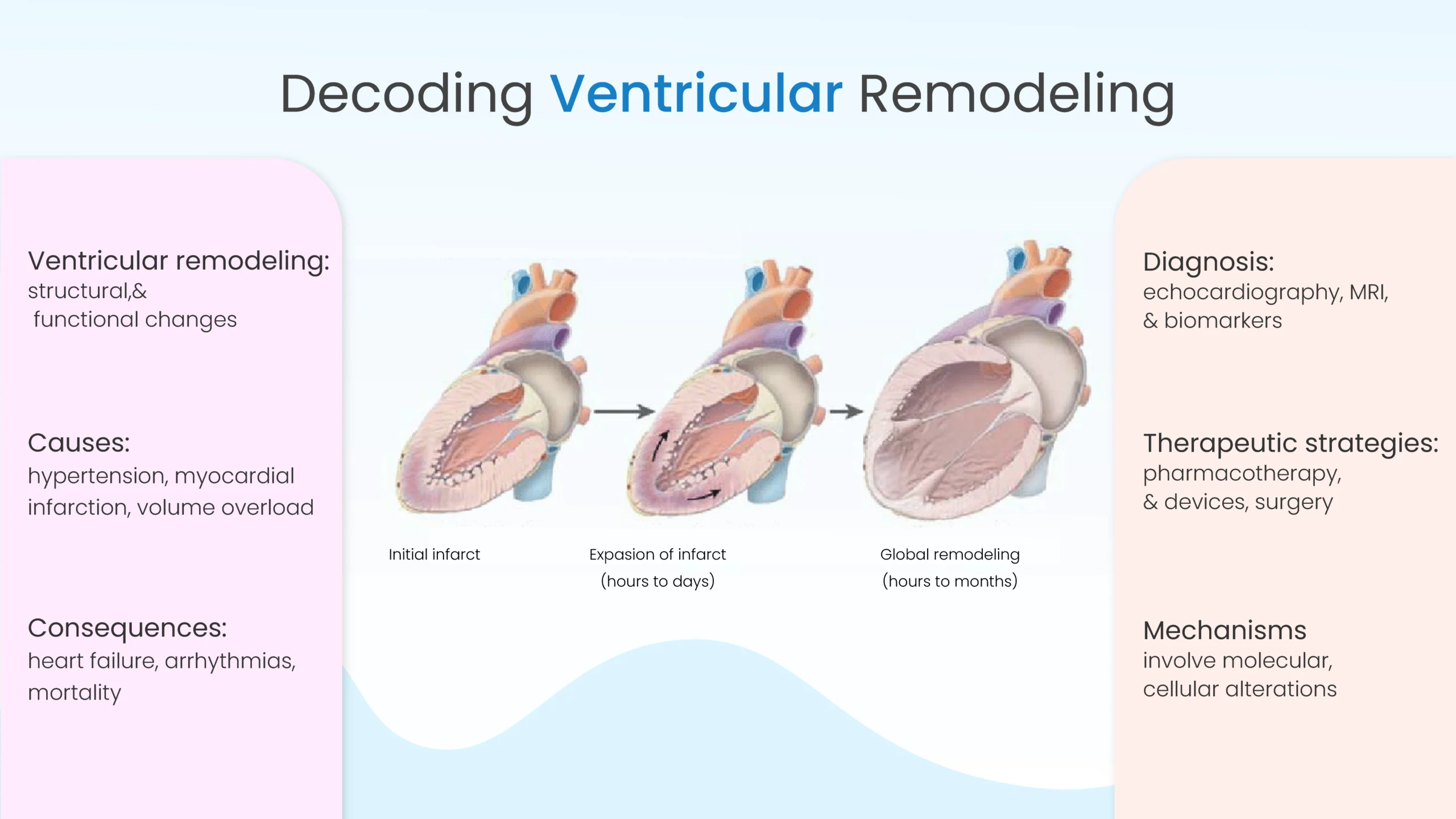
As it is explanatory from its name, ventricular remodeling is associated with the structural and functional changes that occur in the heart’s ventricles; more specifically the left ventricle. These changes occur in response to physiological or pathological stimuli. While ventricular remodeling is typically harmless as it is normally looked upon as a compensatory mechanism the aim of which is to maintain cardiac output, if left unchecked, the condition can lead to dangerous medical complications such as heart failure and the like.
Mechanisms of Ventricular Remodeling
The process of ventricular remodeling is deeply complex. It involves a string of molecular, cellular, and interstitial changes. This condition is triggered by factors such as hypertension, myocardial infarction, or chronic volume overload, remodeling leads to alterations in cardiomyocyte size, shape, and contractility. Apart from this, cardiac fibrosis, characterized by excessive deposition of collagen and other extracellular matrix proteins, further contributes to ventricular stiffening and dysfunction.
Causes of Ventricular Remodeling
As we mentioned earlier, ventricular remodeling can be triggered by several factors, including hypertension, myocardial infarction, and volume overload. Now, let’s learn about these causes in a more detailed and refined manner:
- Hypertension: Persistent elevation in blood pressure imposes increased afterload on the heart, prompting adaptive changes to maintain cardiac output these changes can also cause heart palpitations for a fleeting period of time. However, prolonged hypertensive stress can induce maladaptive remodeling, impairing ventricular function over time.
- Myocardial Infarction: Coronary artery blockage deprives a portion of the heart muscle of oxygen and nutrients, leading to myocardial cell death. The resultant scar tissue formation alters the geometry and contractile properties of the affected ventricle, setting the stage for adverse remodeling.
- Volume Overload: Conditions such as valvular regurgitation associated with valves that prevent the backflow of blood to the heart or chronic anemia can cause an excessive volume load on the heart chambers, triggering compensatory remodeling responses. However, sustained volume overload can overwhelm the heart’s adaptive capacity, resulting in dilated cardiomyopathy and heart failure.
Ventricular Remodeling Consequences
There could be profound implications for ventricular remodeling for cardiac functions and clinical outcomes. As the heart undergoes a structural change in this condition, its ability to pump blood efficiently significantly diminishes. This can lead to several symptoms of heart failure, such as dyspnea, fatigue, and exercise intolerance. Besides this, ventricular remodeling also increases the risk of cardiac arrhythmias of different arrhythmia classifications, thromboembolic events, and sudden cardiac death, imposing significant morbidity and mortality burdens on affected individuals.
Diagnostic Evaluation
Since ventricular remodeling is a deeply intricate condition, its diagnostic evaluation also veers towards the category of complex methods. Early detection of ventricular remodeling is crucial for implementing timely interventions to mitigate its adverse effects. Diagnostic modalities such as echocardiography, cardiac magnetic resonance imaging (MRI), and biomarker assessment (e.g., brain natriuretic peptide) play pivotal roles in evaluating ventricular structure, function, and hemodynamics. These tools enable clinicians to monitor disease progression, assess response to therapy, and stratify patients’ risk for adverse cardiovascular events.
Therapeutic Strategies
Management of ventricular remodeling encompasses pharmacological, device-based, and surgical interventions aimed at addressing underlying etiologies, alleviating symptoms, and improving outcomes. Key therapeutic strategies include:
- Pharmacotherapy: Drugs targeting neurohormonal pathways, such as angiotensin-converting enzyme inhibitors, beta-blockers, and mineralocorticoid receptor antagonists, have demonstrated efficacy in attenuating remodeling and improving survival in heart failure patients.
- Device Therapy: Implantable devices such as cardiac resynchronization therapy (CRT) devices and implantable cardioverter-defibrillators (ICDs) can optimize cardiac function and reduce the risk of life-threatening arrhythmias in select patients with heart failure and ventricular dysfunction.
- Surgical Interventions: Surgical procedures such as coronary artery bypass grafting (CABG) and valve repair or replacement may be indicated in patients with ischemic or valvular heart disease to alleviate hemodynamic burden and prevent further remodeling.
Future Directions
There are many challenges that clinicians face when detecting ventricular remodeling. Despite advances in our understanding and management of ventricular remodeling, its complex nature makes it hard to treat. Further research is needed to unravel the molecular mechanisms driving remodeling processes and identify novel therapeutic targets. Additionally, personalized approaches integrating genomic, proteomic, and imaging data hold promise for optimizing treatment strategies and improving outcomes in patients with ventricular remodeling.
In conclusion, Ventricular Remodeling is a compensatory outcome in a normal scenario that only occurs for the maintenance of cardiac output. However, if this condition grows significantly then it can put a serious dent in your cardiovascular health. Understanding the underlying mechanisms, causes, and consequences of remodeling is essential for guiding clinical decision-making and developing targeted therapeutic interventions. Hence, you must stay vigilant and take utmost care of your heart and ensure that you don’t keep ventricular remodeling untreated.



