Author:- Mr. Ritesh Sharma
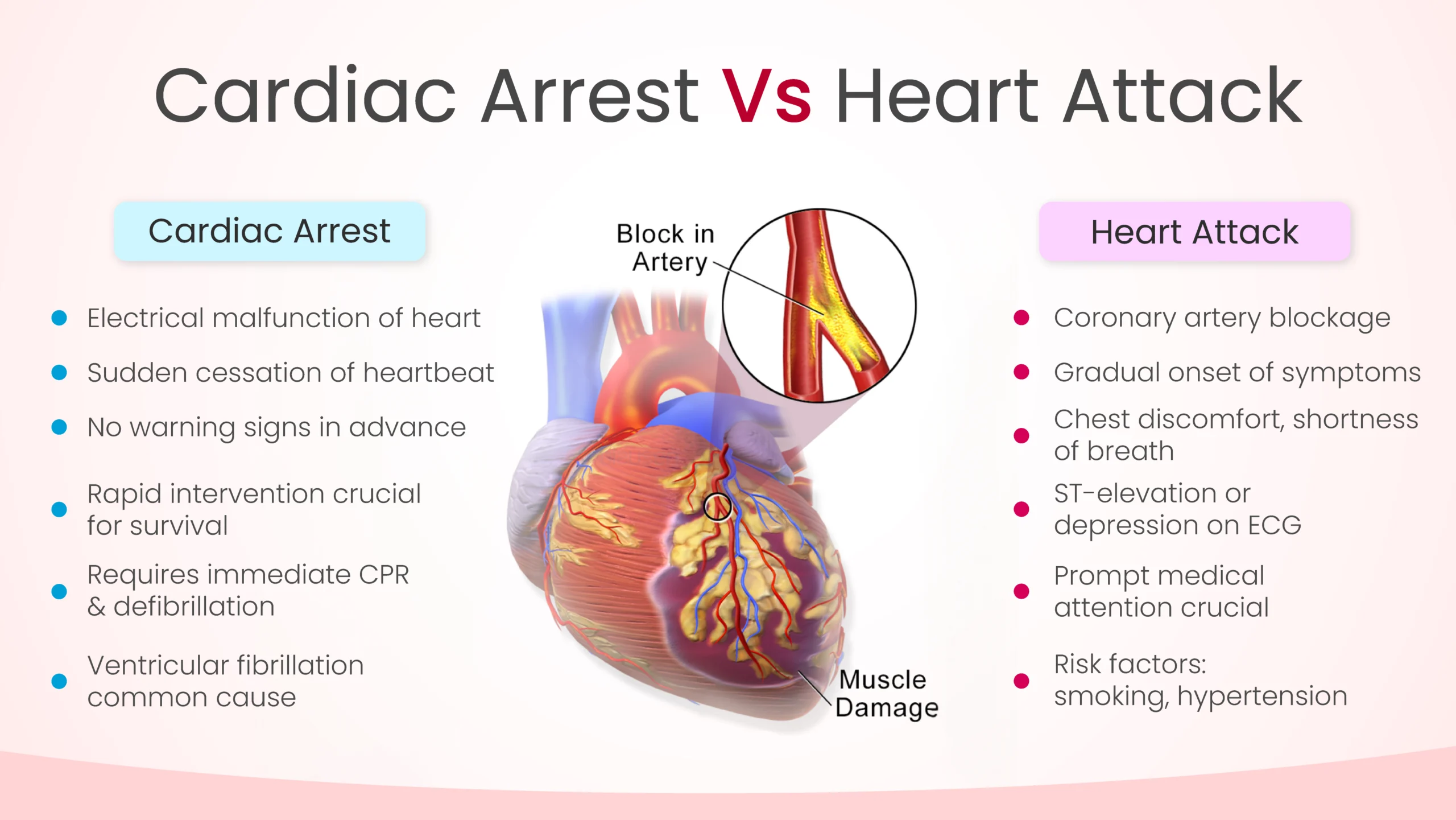
Whether they are general audience or clinicians, the debate of cardiac arrest vs heart attack never fails to intrigue people. These two life-threatening conditions have some similarities albeit many differences that people fail to identify. While cardiac arrest is more associated with the electrical activity of the human heart and its sudden dysfunction, heart attack is more related to the blockage of the coronary circulation. It is important to note that both these conditions pose a serious risk to health and if not treated timely either or both of them can turn out to be fatal.
So, what is cardiac arrest vs heart attack? How do these two conditions related to your heart vary in symptoms, causes, and more? We will examine all this and more in this blog. Therefore, whether you are a clinician or a general audience, get educated and empowered by this blog.
Understanding Cardiac Arrest
To truly understand cardiac arrest vs heart arrest, we will first study the meaning of cardiac arrest. Imagine the heart as the conductor of the body’s orchestra, rhythmically pumping blood to every corner. Now, picture the conductor suddenly dropping the baton, bringing the entire symphony to a screeching halt. This abrupt cessation of heart function characterizes cardiac arrest.
Cardiac arrest occurs when the heart’s electrical system malfunctions, causing it to stop beating effectively. In essence, the heart’s rhythm becomes chaotic or erratic, leading to the cessation of blood flow to vital organs. Without immediate intervention, such as cardiopulmonary resuscitation (CPR) and defibrillation, cardiac arrest swiftly leads to unconsciousness and death within minutes.
One of the striking aspects of cardiac arrest is its sudden onset. Victims may not exhibit any warning signs or symptoms before collapse. However, some individuals may experience chest pain, shortness of breath, dizziness, or heart palpitations moments before cardiac arrest strikes.
Several underlying conditions can precipitate cardiac arrest, including:
- Coronary artery disease (CAD): A condition characterized by the narrowing or blockage of the coronary arteries, reducing blood flow to the heart muscle.
- Cardiac Arrhythmias: Abnormal heart rhythms, such as ventricular fibrillation or ventricular tachycardia, can trigger cardiac arrest.
- Structural heart defects: Certain structural abnormalities of the heart, such as hypertrophic cardiomyopathy, can predispose individuals to sudden cardiac arrest.
Prompt recognition of cardiac arrest and immediate initiation of CPR, along with the use of automated external defibrillators (AEDs), significantly enhance the chances of survival. Every minute without intervention decreases the likelihood of a positive outcome, emphasizing the critical importance of bystander intervention and rapid emergency medical response.
Understanding Heart Attack
Now, let’s move our attention to a heart attack. Heart attack is a condition which is purely associated with coronary arteries (the arteries that supply oxygen-rich blood to the heart). During a heart attack, the coronary arteries get completely blocked due to several reasons, and the heart stops receiving oxygenated blood. Picture a bustling highway where a sudden traffic jam obstructs the flow of vehicles, a similar scenario unfolds within the coronary arteries during a heart attack.
Unlike cardiac arrest, which manifests as a sudden collapse, a heart attack often presents with warning signs and symptoms that may develop gradually, including:
- Chest discomfort: Often described as pressure, tightness, or squeezing in the chest, which may radiate to the arms, back, neck, jaw, or stomach.
- Shortness of breath: Difficulty breathing or feeling breathless, especially with exertion.
- Nausea, indigestion, or abdominal discomfort: Some individuals may experience gastrointestinal symptoms during a heart attack.
- Cold sweat, lightheadedness, or dizziness: These symptoms may accompany chest discomfort or occur independently.
It’s essential to recognize and promptly respond to these warning signs, as early intervention can minimize heart muscle damage and improve outcomes. Seeking emergency medical attention at the first sign of a heart attack is crucial, as timely treatment, such as thrombolytic therapy or percutaneous coronary intervention (PCI), can restore blood flow to the affected artery and prevent further cardiac complications.
Several risk factors contribute to the development of heart attacks, including:
- Smoking: Tobacco use significantly increases the risk of coronary artery disease and heart attacks.
- High blood pressure: Elevated blood pressure puts strain on the heart and damages blood vessels, predisposing individuals to heart attacks.
- High cholesterol: Excess cholesterol can accumulate in the arteries, forming plaques that narrow the vessel lumen and impede blood flow.
- Diabetes: Poorly controlled diabetes can damage blood vessels and nerves, increasing the likelihood of heart attacks.
- Obesity: Excess body weight strains the heart and exacerbates other risk factors, such as high blood pressure and cholesterol levels.
Cardiac Arrest Vs Heart Attack
While cardiac arrest and heart attack are distinct entities, they can sometimes overlap. For instance, a severe heart attack can lead to cardiac arrest if the heart’s electrical system becomes compromised due to extensive myocardial damage. However, recognizing the unique features of each condition is crucial for delivering appropriate interventions and optimizing outcomes. Therefore in the debate of cardiac arrest vs heart attack, this is the sole similarity between the two life-threatening conditions.
Apart from this, to identify cardiac arrest and heart attack, an ECG test is promptly done. In heart attacks, the abnormal ECG will show ST-elevation or ST depression. However, acting more promptly is required in the case of cardiac arrest as any moment can turn out to be fatal for the patient.
In conclusion, cardiac arrest vs heart attack represents two critical cardiac emergencies with distinct etiologies, symptoms, and management strategies. While cardiac arrest involves the sudden cessation of heart function due to electrical abnormalities, a heart attack occurs when a coronary artery becomes obstructed, leading to myocardial ischemia. Timely recognition, prompt intervention, and access to emergency medical care are essential for improving survival rates and minimizing long-term complications associated with these life-threatening events. By understanding the differences between cardiac arrest and heart attack, individuals can empower themselves to take proactive steps toward heart health and potentially save lives in the process.





